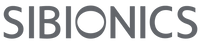
5 Ways Sleep Affects Your Blood Glucose Levels
Sleep is often hailed as the unsung hero of good health, influencing everything from mood to cognitive function. But did you know that it also plays a significant role in regulating your blood glucose levels? Yes, the quality and quantity of your sleep can significantly impact how your body manages glucose, the primary source of energy. In this article, let's explore five ways that sleep affects your blood glucose:
1. Insulin Sensitivity:
One of the key mechanisms through which sleep influences your blood glucose levels is insulin sensitivity. Adequate sleep helps maintain optimal insulin sensitivity, allowing cells to efficiently respond to the insulin signals to take up glucose from the bloodstream. However, when sleep is inadequate or disrupted, as seen in sleep conditions like Obstructive Sleep Apnea Syndrome(OSAS) or chronic insomnia, insulin sensitivity decreases. This reduced sensitivity can lead to insulin resistance, where cells become less responsive to insulin, resulting in elevated blood glucose levels.
2. Hormonal Imbalance:
Sleep deprivation can disrupt your body’s delicate balance of hormones involved in blood sugar regulation. Research indicates that insufficient sleep can elevate cortisol levels the next morning, a stress hormone known to impair insulin action. Moreover, inadequate sleep is associated with alterations in appetite-regulating hormones, such as decreased leptin and increased ghrelin levels. These hormonal imbalances can lead to overeating, weight gain, and ultimately, worsened blood sugar control.
3. Nocturnal Glycemic Control:
Sleep disturbances can also impact nocturnal blood glucose levels, affecting overall glycemic control. Individuals with sleep disorders are more likely to experience fluctuations in blood sugar levels during sleep, characterized by periods of nocturnal hypoglycemia followed by rebound hyperglycemia. These frequent blood sugar fluctuations disrupt sleep patterns and pose further risks for long-term metabolic health. It has been suggested that sleep deprivation might causally contribute to the development of obesity and type 2 diabetes. The metabolic influence mechanism is depicted as follows:

Metabolic pathways linking sleep disorders with the development of Type 2 diabetes
Image Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4381534/
4. Glucose Metabolism:
Sleep plays a vital role in regulating glucose metabolism, the process by which the body processes and utilizes glucose for energy. A study that investigated whether sleep extension in chronically sleep-deprived individuals would improve glucose metabolism, also suggested that an objectively-extended amount of sleep could benefit metabolic health. Several well-constructed sleep restriction experiments have also confirmed that sleep deprivation can impair glucose metabolism, which could lead to decreased glucose uptake by tissues and increased glucose production by the liver. These alterations in glucose metabolism eventually would contribute to elevated blood glucose levels and insulin resistance.
5. Lifestyle Factors:
Beyond direct physiological mechanisms, sleep also influences lifestyle factors that impact blood glucose levels. For instance, insufficient or poor sleep often increases cravings for sugary and high-carbohydrate foods, as well as decreases motivation for physical activity. These behavioral changes can contribute to poor dietary choices, weight gain, and impaired glucose metabolism over time.

Image Source: https://news.uga.edu/avoid-overeating-working-from-home/
Sleep Tips for Better Glucose Management:
Given the intricate relationship between sleep and blood glucose regulation, prioritizing quality sleep is paramount for overall health and well-being. Here are some tips to enhance your sleep hygiene and support optimal blood glucose control:
- Maintain a Consistent Sleep Schedule: Aim for seven to nine hours of quality sleep each night, and try to go to bed and wake up at the same time every day, even on weekends.
-
Create a Relaxing Bedtime Routine: Wind down before bed by engaging in calming activities such as reading, meditation, or gentle yoga stretching. Minimize exposure to blue lights, screens, and stimulating content at least an hour before bedtime.
-
Optimize Your Sleep Environment: Create a sleep-conducive environment by keeping your bedroom relatively cool, dark, and quiet. If possible, invest in a comfortable mattress and pillows to promote restful sleep.
-
Limit Stimulants and Heavy Meals Before Bed: Avoid caffeine and heavy, spicy, or oily foods close to bedtime, as they can disrupt sleep and exacerbate reflux symptoms.
-
Review Your Nighttime Glucose Patterns: Wear a continuous glucose monitoring sensor like the GS1, which offers real-time glucose monitoring and generates comprehensive daily glucose reports for you to review and improve your blood glucose management.
- Seek Professional Help if Needed: If you're struggling with chronic sleep problems or suspect an underlying sleep disorder, consult a sleep coach, or healthcare provider for a comprehensive evaluation and more personalized treatment plan.
Conclusion:
The relationship between sleep and blood glucose regulation is intricate and multifaceted. By understanding how sleep affects insulin sensitivity, hormonal balance, glycemic control, glucose metabolism, and behaviors, we can appreciate the importance of prioritizing quality sleep for glucose management and overall metabolic health.
If you're struggling to achieve restful sleep or experiencing difficulties with glucose management, try following the sleep-promoting tips mentioned in this article, and consider consulting with a healthcare provider or sleep specialist when needed. By addressing sleep disturbances and adopting healthy sleep habits, you can optimize your blood glucose control and promote overall well-being. Remember, sleep isn't just downtime – it's a critical component of a healthy lifestyle.
FAQ:
Q: Does sleep quality matter for glucose control?
A: Yes, sleep quality matters. Restorative sleep, characterized by uninterrupted sleep cycles and adequate time spent in deep sleep stages, is essential for proper glucose regulation. Poor sleep quality, such as frequent awakenings or sleep disorders like sleep apnea, can impair glucose metabolism.
Q: How does the circadian rhythm influence glucose control during sleep?
A: The circadian rhythm, or the body's internal clock, regulates various physiological processes, including glucose metabolism. It dictates the timing of hormone release, such as insulin and cortisol, which are crucial for glucose control. Disruptions to the circadian rhythm, such as shift work or irregular sleep schedules, can adversely affect glucose regulation.
Q: Can improving sleep habits help manage diabetes?
A: Yes, improving sleep habits can positively impact diabetes management. Consistent, sufficient, and high-quality sleep can enhance insulin sensitivity and promote better glucose control. Strategies for improving sleep may include maintaining a regular sleep schedule, creating a sleep-conducive environment, managing stress, and addressing sleep disorders if present.
Q: How does sleep deprivation affect insulin sensitivity?
A: Sleep deprivation can lead to decreased insulin sensitivity, making it more difficult for cells to respond to insulin and regulate blood sugar levels effectively. This can contribute to the insulin resistance and increase the risk of type 2 diabetes.
References:
https://pubmed.ncbi.nlm.nih.gov/9415946/